We know that myopia progression is an increasingly prominent issue with long-term risks to sight. We know that lifestyle is a key driver in myopia development.
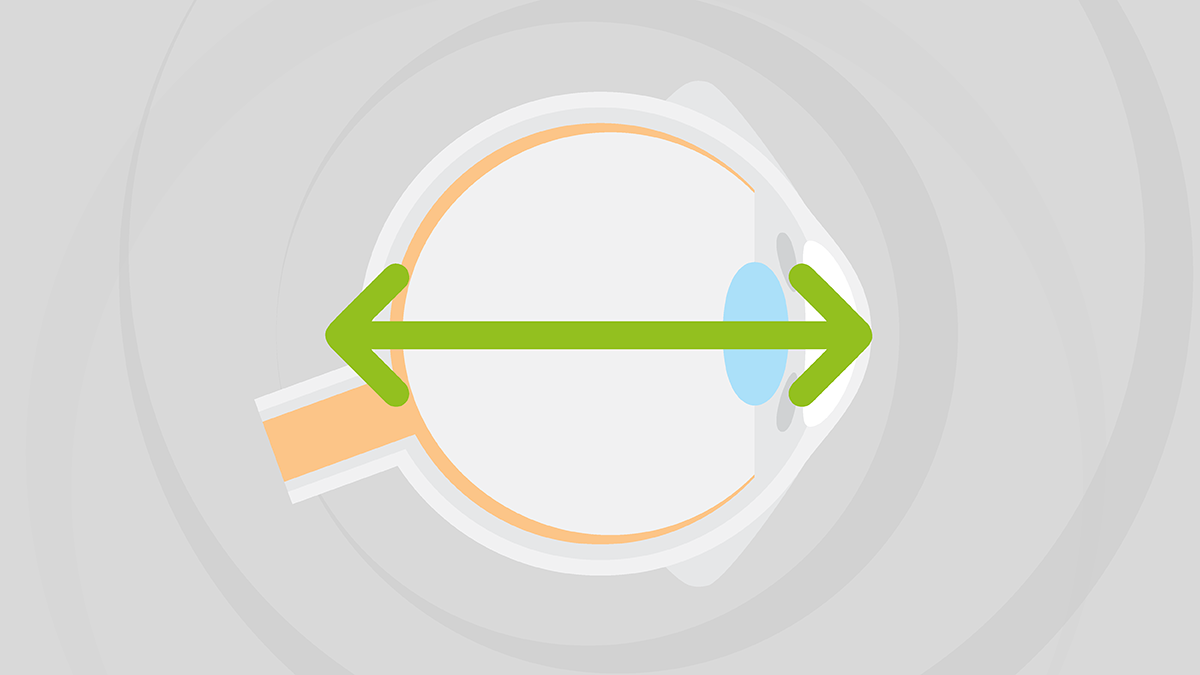
We also know that most myopia is axial myopia.
The myopic refractive error does not always accurately represent the level of risk a patient has in developing sight threatening complications later in life. Axial length, however, is more directly proportional to patients’ future risk of sight-threatening conditions.
When we intervene with myopia management therapies, we’re trying to reduce axial elongation, directly or indirectly. So perhaps it is time to rename myopia management – how does everyone feel about “axial length management?!”
There are those who will argue that refraction is just as effective a tool for diagnosing and monitoring myopia. And there are, of course, multiple reasons why measuring the refractive error is vitally important. However, it’s also important that cycloplegic refraction takes place in myopia management. But this is more time-consuming and generally not pleasant for young children. It also requires the use of single-use minims and creates plastic waste. And despite the optometrist’s skills, the results of refractions will likely vary more than axial length measurements.
If you use orthokeratology (ortho-k) as a therapy in myopia management, you won’t be able to measure the patient’s refraction. You could use an over-refraction measure (maybe even cycloplegic), but again this is less reliable, less repeatable, and less accurate.
Measuring axial length? Well, it is ideal for follow up appointments and it is reliable, repeatable, and generally easy.

Several years ago, I ran a CPD webinar on commercializing myopia management and asked delegates to complete some poll questions. Around 95 percent of the 600 optometrists and clinicians in attendance said they wanted to engage in myopia management or were already doing so. However, 94 percent said they had no means of measuring axial length. This is something of a problem if axial length is to become the definitive measure in myopia management.
The College of Optometrists considers axial length measurement of primary importance, but at present it’s more a “nice to have” than a necessity. Other bodies, such as the International Myopia Institute and the World Council of Optometry (WCO), also advocate axial length measurement as a key part of myopia management, but there is still no widespread axial length management availability in most countries.
But in speaking to many key individuals engaged in myopia management, the consensus seems to be:
- If you are going to seriously engage in myopia management in practice and fully understand the initial and long-term risks to patients – as well as better understand the predictions of untreated versus treated axial length – then measuring axial length is essential.
- It is axial length that “does the damage” – if you don’t measure this, you can never be sure of the predicted risk before, during, and even after myopia management.
- One of the most effective therapies so far is ortho-k – and axial length is an essential measurement if you’re going to offer this treatment.
It’s clear that the debate about making axial length the primary measure in myopia management has begun. One major argument in favor of refraction is that optometrists are already doing it and don’t need to invest in any further equipment. However, there is also a medico-legal argument in favor of axial length measurement. The WCO published a resolution on the standard of care for myopia management, which defines the evidence-based standard of care as comprising three main components: mitigation, measurement, and management. Measurement is defined as “optometrists evaluating the status of a patient during regular comprehensive vision and eye health exams, (e.g., refractive error and axial length whenever possible).” Further, WCO advises optometrists:
“to incorporate the standard of care for myopia management within their practice that shifts from not only correcting vision, but includes public education and early and frequent discussions with parents that explains:
- what myopia is
- lifestyle factors that may impact myopia
- the increased risks to long-term ocular health that myopia brings
- the available approaches that can be used to manage myopia and slow its progression.”
Something perhaps missing from the above is protecting the profession legally. The “cat is out of the bag” as far as myopia is concerned. It is not an option for optometrists to do nothing. And, in my opinion, it’s also not an option to do the minimum.
There could come a time when former child patients seek legal advice if they feel they were not advised correctly about myopia and its risks. Furthermore, they may feel their myopia management was substandard or not enough was done to help them. Whether or not this argument is valid, the more measurements, assessments, and history-taking you do as an optometrist – with effective note-taking – the better. Axial length measurements will likely strengthen your evidence-based practice and provide assurance that what you’re doing is the very best for your patient.
Find out more at myopiafocus.org

