A large-scale, prospective cohort study identified multiple modifiable risk factors associated with sudden cardiac arrest and quantified their population-attributable burden using an exposome-wide association study and Mendelian randomization. The findings suggested that interventions targeting unfavorable lifestyle, physical, psychosocial, socioeconomic, and environmental profiles could substantially reduce incident sudden cardiac arrest risk.
Study Overview
Investigators from Fudan University analyzed data from 502,094 participants in the UK Biobank cohort who were followed for a median of 13.8 years. During this period, 3,147 individuals developed sudden cardiac arrest (SCA). A total of 125 potentially modifiable exposures were assessed across six domains: lifestyle, physical measures, psychosocial factors, socioeconomic status, local environment, and early-life exposures.
Exposome-wide association study (EWAS) models that were adjusted for age, sex, race, and assessment center identified 56 nonclinical risk factors significantly associated with incident SCA. Mendelian randomization (MR) analysis was subsequently conducted to assess causality using genome-wide association study (GWAS) data from independent samples.
Causal Risk and Protective Factors
Among the 56 risk factors identified in the EWAS, MR analysis supported 9 causal associations:
Protective factors (inverse association with SCA):
-
Higher dried fruit intake
-
Greater champagne/white wine consumption
-
Time spent using a computer (noted as directionally inconsistent across analyses).
Adverse factors (positive association with SCA):
-
Fed-up feelings
-
Higher body mass index
-
Greater arm fat mass and percentage
-
Elevated systolic blood pressure
-
Lower education level (as indicated by having no qualifications).
Although computer use showed an inverse association in EWAS, MR findings were inconsistent in direction and should be interpreted cautiously.
Population Attributable Burden
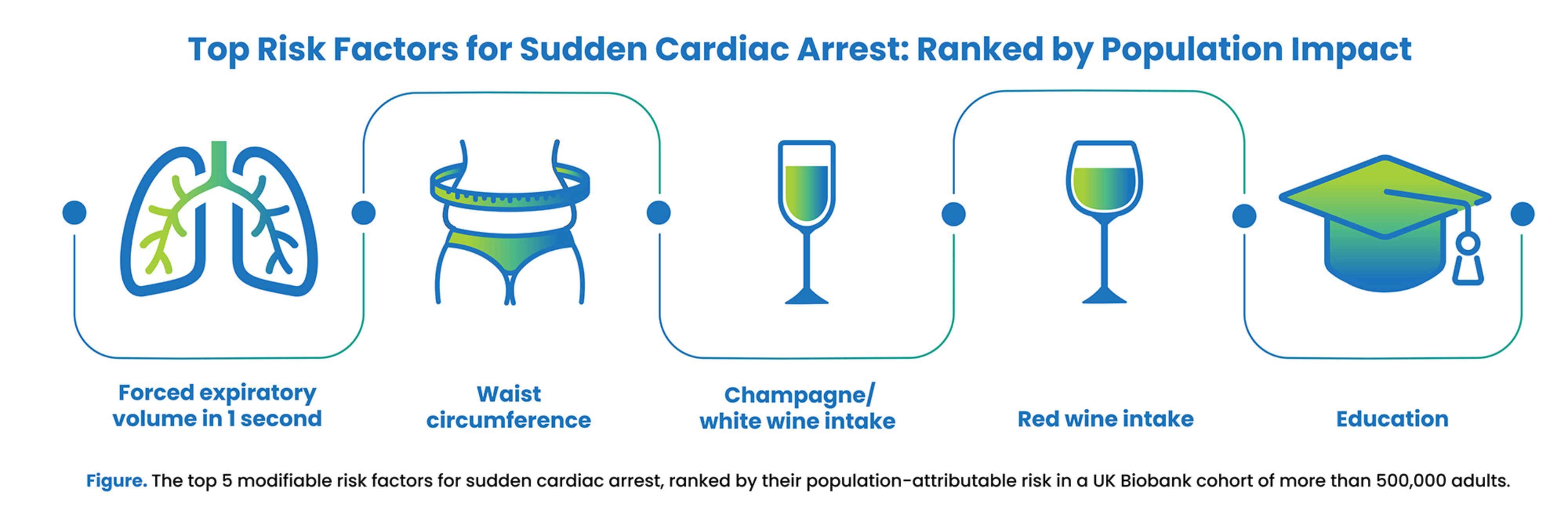
Forced expiratory volume in 1 second was identified as the single largest risk factor, accounting for 24.7% of SCA cases. An additional 25 risk factors had population attributable fractions (PAF) ranging from 10.0% to 17.4%, including tobacco use, physical inactivity, sleep disturbances, and low educational attainment.
By aggregating PAFs within each domain and adjusting for overlapping factors using weighted estimates, the investigators determined:
-
40% of SCA cases could be prevented through conservative elimination of the most unfavorable profiles (worst third).
-
63% of cases could be prevented through thorough elimination of both unfavorable and intermediate profiles.
Preventive Potential by Domain
-
Lifestyle: 13%–18%
-
Physical measures: 9%–14%
-
Socioeconomic status: 8%–10%
-
Psychosocial factors: 5%–14%
-
Local environment: 5%–7%.
Methodology
The researchers employed a hypothesis-free, data-driven EWAS framework followed by MR validation. GWAS summary statistics were sourced for exposures and outcomes to test causality using inverse variance weighting as the primary MR method, with MR Egger and weighted median models for sensitivity analyses. Population attributable risks were calculated using prevalence-adjusted statistical models with communality correction to avoid overestimation as a result of overlapping exposures.
Limitations
The study acknowledged several limitations:
-
The UK Biobank population consisted predominantly of White, middle-aged to older adults, which may have limited generalizability.
-
Some SCA cases may have been misclassified because of the reliance on administrative records, potentially leading to attenuated associations.
-
Not all exposures of interest could be evaluated as a result of data availability or instrument strength in MR.
-
Results don't distinguish between out-of-hospital and in-hospital SCA or between shockable and nonshockable rhythms.
Conclusion
This study was among the first to combine EWAS and MR to comprehensively evaluate the modifiable risk profile of SCA in a large, prospective cohort. The results underscored the potential for prevention through public health strategies, particularly those addressing lifestyle, socioeconomic, and psychosocial factors.
Source: Canadian Journal of Cardiology
