
In my dry eye referral practice, all patients have moderate to severe dry eye disease (DED), and artificial tears are always part of the management plan. In their search for relief, most of my patients have tried three to five different brands of artificial tears and come away frustrated when they don’t help. In fact, some patients have chosen eye drops that make their DED worse. Recently, a woman presented with severe punctate keratitis, the result of excessive use of a redness-reducing drop preserved with BAK that she assumed was the same as artificial tears. I had to treat her with an amniotic membrane.

These problems are understandable – there are many options in the eye care aisles, and patients don’t know what ingredients to avoid. To make it more confusing, attractive marketing terms like “severe dry eye,” “soothing,” and “natural” are printed on some products that aren’t necessarily the best for their specific needs. To ensure patients get the right tears to help manage DED, we need to do two things: i) educate them about the ingredients in artificial tears, and ii) tell them the specific tear that we want them to purchase.
Seeking out ingredients
I tell patients that we choose better ingredients for their eyes, just like we choose better ingredients when we buy groceries. Bargain eye drops are like powdered milk: they cost less, but it’s well worth paying a few more dollars to get the real thing.
I educate patients about two basic ingredients in artificial tears, as well as a few additions contained in some products. First, most artificial tears contain a viscosity agent to make the drops thicker and help them retain water on the ocular surface. I choose drops with viscosity agents that the literature has shown offer protective benefits as well:
- Hyaluronic acid (HA) (sodium hyaluronate). I’m a huge fan of HA, which is both a viscosity agent and an antioxidant. HA has been shown to accelerate healing on the ocular surface (1), which I think makes it ideal for helping patients counteract the desiccating stress of DED.
- Carboxymethylcellulose (CMC). CMC has a lower residence time on the eye than HA (2), but it’s another good viscosity agent that protects the corneal surface and promotes wound healing (3).
A new trend in artificial tears is the addition of two other ingredients that can help protect the ocular surface:
- Trehalose. This ingredient helps protect epithelial cells, reduce osmolarity, stabilize the tear film’s lipid layer, and provide anti-inflammatory action (4).
- Glycerin. This lubricant is also an osmoprotectant that can reduce hyperosmolarity and cell damage to the ocular surface (5).
Finally, I tell my patients to choose tears that say “preservative-free” on the box. Advances in bottle technology have made it safe to store preservative-free tears in multi-dose bottles, so patients can get a bottle they like instead of the little vials that they may have found frustrating in the past.
Following the recommendations
Educating patients about ingredients helps them understand why we’re recommending a certain tear or switching them off their old artificial tears. Even after we recommend a specific tear, they can use this information to find a healthy alternative if they’re limited to shopping someplace that doesn’t carry their usual tears (while on vacation, for example).
With the ingredients and benefits in mind, my first choice is a preservative-free tear with povidone (a lubricant), HA, and trehalose called iVizia (Thea). It has the ingredients I want, it’s preservative-free, and it’s the most popular with my patients based on the results they’re getting. iVizia also has a bottle that’s a little easier to use than some of the designs for preservative-free tears. My other preservative-free options are a carboxymethylcellulose and glycerin formulation called Refresh Relieva PF (Allergan) and a tear with HA and glycerin called Optase Dry Eye Intense Drops (Scope). Both of these tears also come in multi-use bottles.
I also keep an open mind to using other tears based on a patient’s individual situation. For example, I sometimes use artificial tears that contain oil for patients with meibomian gland dysfunction (MGD) and those with severe combination DED until I can restore their own oil production with other MGD therapies, such as thermal pulsation and intense pulsed light (IPL). I tell patients to look for the word “oil” on the ingredients list of a preservative-free tear, and I recommend a specific option, such as Optase MGD Advanced (Scope) or Refresh Optive Mega-3 (Allergan). (Note: These drops cannot be used with contact lenses.)
Because I only treat moderate to severe DED, I see many patients with lagophthalmos who need overnight support. There is a trend of adding antioxidants and various oils to the traditional combination of paraffin and mineral oil. My patients are having success with the combination of eyelid stickers (SleepTite/SleepRite) and Optase Hylo Night ointment (Scope), which has vitamin A to support corneal integrity (6). For patients who can’t tolerate or don’t like ointment, I recommend using eyelid stickers with the HA/trehalose formulation of iVizia Lubricant Eye Gel for Severe/Night Dry Eyes (Thea). These therapies protect and moisturize the eyes at night, so patients with lagophthalmos don’t wake with a deficit that we can’t overcome.
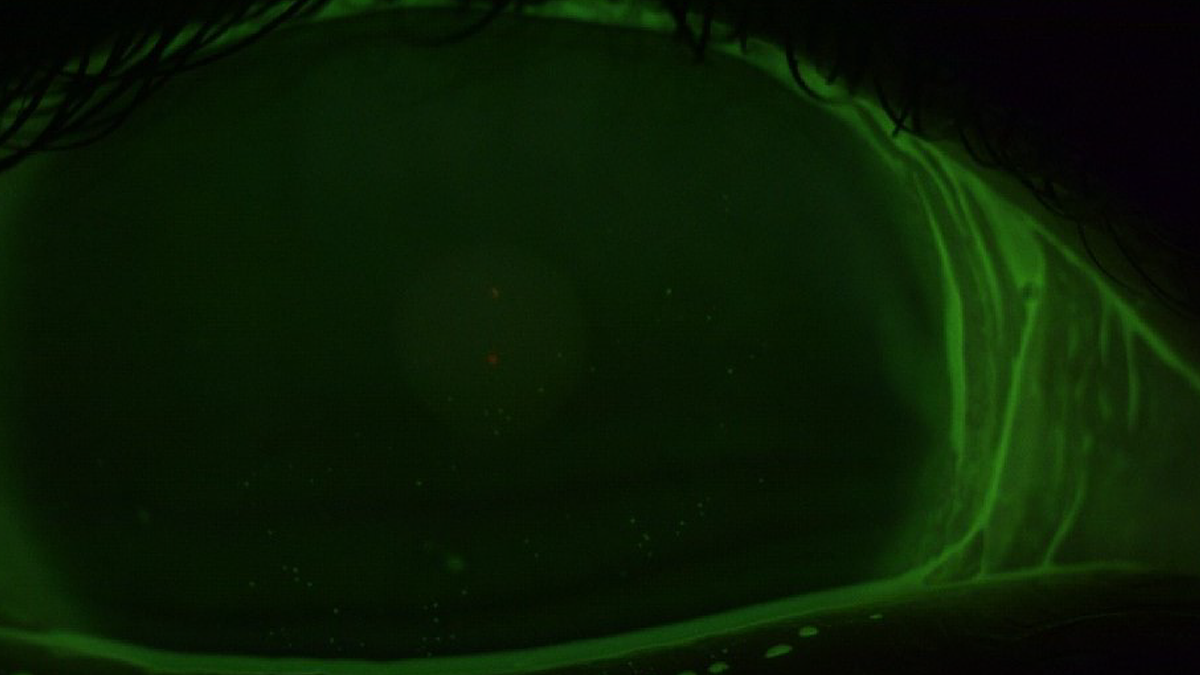
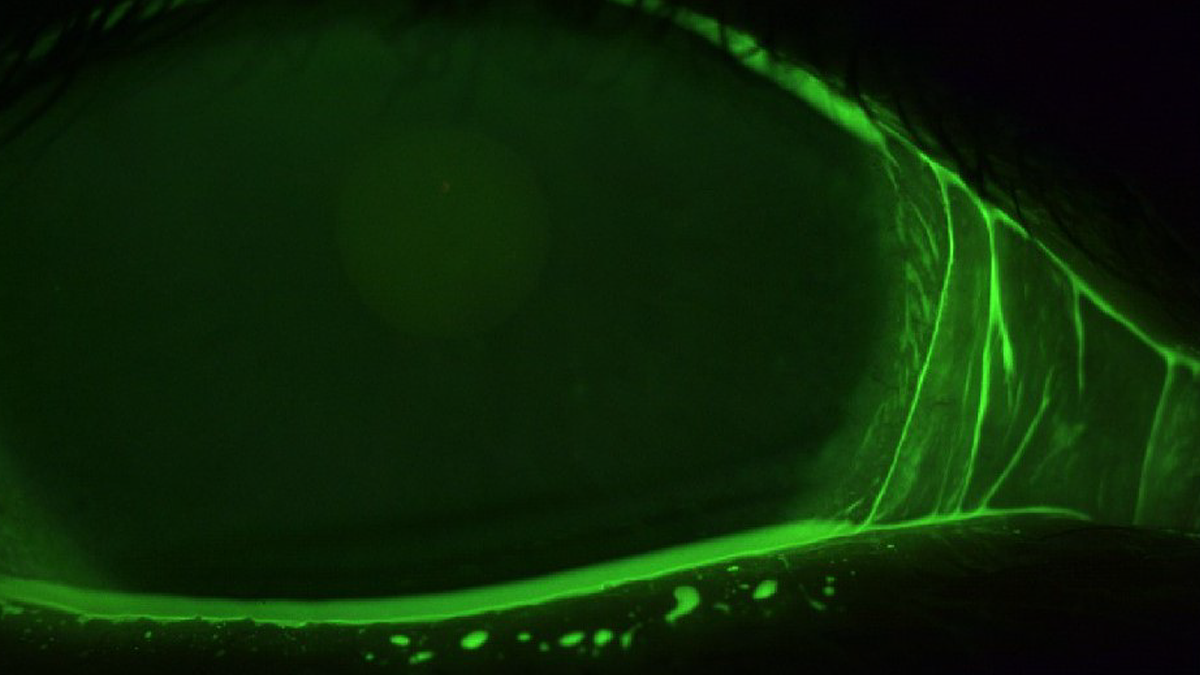
Figures 1 & 2. Before and after treatment. Note the improvement in lower corneal fluorescein staining with the addition of quality preservative-free tears. (Figure 1. Before treatment. Figure 2. After treatment.) (Credit: Images supplied by author)
Finally, electrolytes are also included in some artificial tears, as they help mimic the composition of natural tears. Electrolytes aid in maintaining the osmotic balance of the ocular surface, which is crucial for eye health (7). Recall that “hyperosmolarity” is included in the definition of dry eye by DEWS II (8). Common electrolyte ingredients seen in artificial tears are sodium, potassium, chloride, magnesium, and calcium.
Case study: Saving a contact lens dropout
A 46-year-old woman came in for our first visit and told me, “I can’t wear contact lenses anymore – my eyes feel terrible!” Her paperwork showed she was likely experiencing hormonal changes, and she had well-controlled diabetes. We discussed lifestyle factors, and I learned that she’d stopped wearing eye make-up and typically spent about eight hours per day using a computer. The patient’s workup showed she had MGD, mild ocular rosacea, and inflammation evidenced by punctate epithelial erosions.
I started her with regular use of Ivizia daytime tears (morning, afternoon, night, and as needed) and okra-based lid hygiene (ZocuFoam, Zocular). She returned two weeks later for an IPL series, followed by thermal meibomian gland expression. Her eyes had already begun to feel mildly better within those two weeks due to the regular tear use and lid scrubs. Once her in-office therapies were complete, reducing inflammation and allowing her to produce a healthier tear film, she was able to go back to wearing daily contact lenses comfortably. iVizia tears are compatible with contact lenses, so she continued to use them as needed, usually 1x midday at her computer for preventative ocular surface protection.
The patient hit a snag when she ran out of daily lenses. She couldn’t afford more, so she went back to her stock of the less expensive two-week lenses she’d worn in the past. Her eyes could not tolerate these two-week lenses for more than four hours. I instructed her to go back to using iVizia on a schedule of 2–3 times per day. She found that she can comfortably wear the less expensive two-week lenses for most of the day as long as she uses her artificial tears as instructed. She does plan to reorder dailies once she works through her two-weeks lenses, but right now the patient is happy. She’s using her computer all day and wearing makeup again with the right artificial tear and the right ingredients for her situation – something all DED patients can enjoy.


Figures 3 & 4. Before and after treatment; clearing of cylindrical dandruff with okra-based lid hygiene. (Credit: Images supplied by author)
- JA Gomes et al., “Sodium hyaluronate (hyaluronic acid) promotes migration of human corneal epithelial cells in vitro,” Br J Ophthalmol., 88, 821 (2004). doi:10.1136/bjo.2003.027573.
- X Zheng et al., “Comparison of in vivo efficacy of different ocular lubricants in dry eye animal models,” Invest Ophthalmol Vis Sci., 55, 3454 (2014). doi:10.1167/iovs.13-13730.
- Q Garrett et al., “Carboxymethylcellulose binds to human corneal epithelial cells and is a modulator of corneal epithelial wound healing,” Invest Ophthalmol Vis Sci., 48, 1559 (2007). doi:10.1167/iovs.06-0848.
- A Ballesteros-Sánchez et al., “Trehalose and Dry Eye Disease: A Comprehensive Systematic Review of Randomized Controlled Trials,” J Clin Med., 12, 7301 (2023). doi:10.3390/jcm12237301
- C Lievens et al., “Evaluation of an enhanced viscosity artificial tear for moderate to severe dry eye disease: A multicenter, double-masked, randomized 30-day study,” Cont Lens Anterior Eye, 42, 443 (2019). doi:10.1016/j.clae.2018.12.003.
- C Samarawickrama, “Retinoic acid and the ocular surface,” Surv Ophthalmol., 60, 183 (2015). doi: 10.1016/j.survophthal.2014.10.001. Epub (2014). PMID: 25890622.
- M Labetoulle et al., “Artificial Tears: Biological Role of Their Ingredients in the Management of Dry Eye Disease,” Int J Mol Sci., 23, 2434 (2022). doi: 10.3390/ijms23052434. PMID: 35269576.
- F Stapleton et al., “TFOS DEWS II Epidemiology Report,” Ocul Surf., 15, 334 (2017). doi:10.1016/j.jtos.2017.05.003.





