A 37-year-old woman developed pneumomediastinum and subcutaneous emphysema following a routine dental cleaning procedure with a high-pressure air-water device, according to a case report.
The patient experienced sudden-onset tearing pain in her jaw several minutes into a dental cleaning performed with a high-pressure stream of water, air, and cleaning powder, followed by progressive facial, neck, and chest swelling, dyspnea, and chest pain.
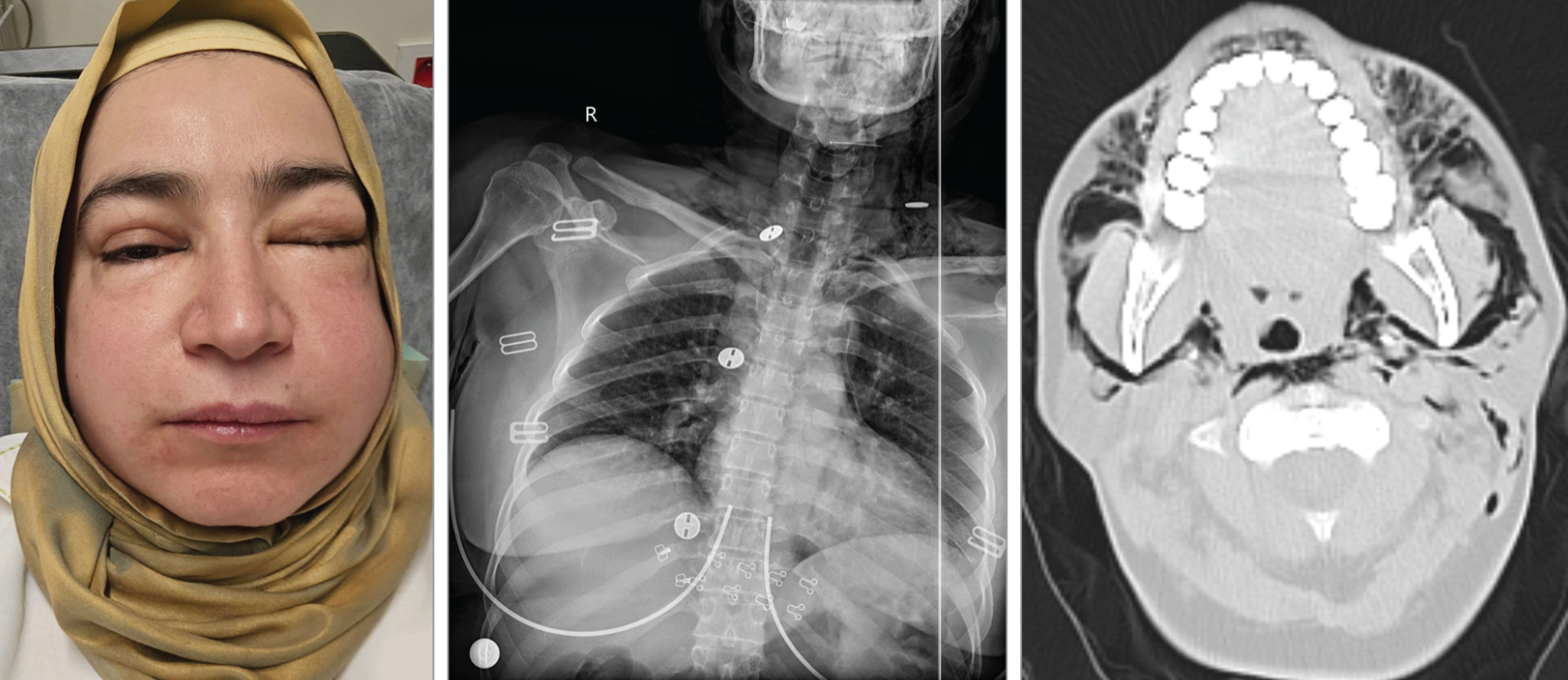
Physical examination revealed facial swelling and palpable subcutaneous crepitus over her anterior chest wall, neck, and periorbital region. Her vital signs showed blood pressure of 110/70 mmHg, pulse rate of 130 per minute, respiration of 25 per minute, and oxygen saturation of 92% while breathing room air. Chest radiography and computed tomography (CT) showed air located in the subcutaneous tissues of the face and neck and in the fascial planes of the neck and mediastinum.
Treatment and Management
The patient initially received oxygen via a face mask at 6 L per minute, intravenous dexamethasone (8 mg), intravenous acetaminophen (1,000 mg), as well as nebulized ipratropium bromide (0.5 mg), salbutamol (2.5 mg), and budesonide (1 g). High-flow oxygen therapy was the appropriate next step in management.
"The key to the correct answer is recognizing that pneumomediastinum and subcutaneous emphysema are typically self-limited conditions that may resolve more rapidly with oxygen therapy," the study authors wrote. "High-flow oxygen therapy can enhance resorption of mediastinal air by increasing the alveolar partial pressure of oxygen, creating a diffusion gradient that promotes the displacement of nitrogen from the mediastinal air pocket, leading to faster resolution of pneumomediastinum," they added.
Other management approaches, including bronchoscopy, mediastinal drainage, and needle decompression weren't indicated for this patient. Bronchoscopy isn't recommended because the patient had no evidence of major airway trauma. Mediastinal drainage is reserved for airway perforation, esophageal rupture, or severe progressive respiratory distress. Needle decompression isn't indicated because the patient didn't have a tension pneumothorax.
Mechanism and Risk Factors
"High-pressure dental airflow devices, including air-powder polishers, high-speed drills, and air-water syringes generate strong jets of air and water that can track into subcutaneous and mediastinal tissues through small defects in the gingival or mucosal surfaces, causing pneumomediastinum," the study authors noted.
The case highlighted risk factors for this rare complication:
"The incidence of pneumomediastinum due to dental air and water flow devices is rare. Case series report that patients at higher risk include those undergoing prolonged dental procedures with air-driven tools, individuals with chronic corticosteroid use or connective tissue disorders, and those undergoing mandibular third molar extraction," the study authors detailed. They also suggested that directing high-pressure air into gingival pockets or open wounds increases risk.
Clinical Presentation and Diagnosis
"Patients with pneumomediastinum typically present with chest pain, dyspnea, and neck pain. Subcutaneous emphysema occurs in approximately 35% of patients with pneumomediastinum. Hamman sign—a crunching or bubbling sound heard during cardiac auscultation—is identified in 5.9% of patients with pneumomediastinum, and concurrent pneumothorax occurs in approximately 5.2%," the study authors indicated.
While chest radiography is typically the initial diagnostic imaging study, its sensitivity for identifying pneumomediastinum ranges from 61% to 100%. Chest CT is the criterion standard for diagnosis and should be obtained in patients clinically suspected of having pneumomediastinum that isn't identified on chest radiograph.
Potential Complications
"Rare complications of pneumomediastinum include tension pneumomediastinum, mediastinitis, pneumoperitoneum, pneumopericardium, and pneumorrhachis (air within the spinal canal). Tension pneumomediastinum occurs if increased air pressure within the mediastinum compresses the trachea and major blood vessels, reducing venous return and decreasing cardiac output. Treatment involves immediate decompression of the mediastinum with needle aspiration, placement of a chest tube, or surgery (emergent anterior subxiphoid incision)," the study authors continued.
Mediastinitis typically presents with fever, increased chest pain, and odynophagia and is treated with thoracoscopic drainage and broad-spectrum antibiotics.
Patients with pneumomediastinum should be hospitalized for close monitoring and supportive care if they have chest pain, respiratory distress, hemodynamic instability, hypoxemia, rapidly worsening subcutaneous emphysema, tension pneumomediastinum, pneumomediastinum with lung disease, or suspected esophageal perforation. Patients with mild, stable pneumomediastinum based on clinical findings and vital signs may be discharged from the emergency department with follow-up evaluation in 24 to 48 hours.
Patient Outcome
"The patient was admitted to the thoracic surgical service and received oxygen by nasal cannula (6 L per minute) and nonsteroidal anti-inflammatory analgesia (dexketoprofen [50 mg/2 mL], intramuscularly twice daily). Daily chest radiography demonstrated a gradual decrease in pneumomediastinum and subcutaneous emphysema. On hospital day 4, she was asymptomatic and was discharged. Two months after discharge, her chest radiograph was normal," the study authors concluded.
The patient was advised to avoid high-pressure air and water devices during future dental cleanings to reduce recurrence risk.
Which option would you select?
A. Administer high-flow oxygen therapy
B. Evaluate for endobronchial injury with emergency bronchoscopy
C. Initiate surgical decompression with mediastinal drainage
D. Perform needle decompression thoracostomy
Source: JAMA Clinical Challenge
