Variants of uncertain significance (VUS) continue to complicate the interpretation of diagnostic genetic tests, and experts are intensifying efforts to reduce their prevalence. Speaking at the Association for Molecular Pathology (AMP) annual meeting in Boston, Heidi L. Rehm, PhD, of Massachusetts General Hospital and the Broad Institute of MIT and Harvard, outlined practical strategies for resolving VUS, describing the predominance of these inconclusive results as one of the “biggest challenges to precision genomic medicine.”
“About one-third of all symptomatic genetic tests end with a VUS, which has a huge clinical impact on patients, physicians, and our field,” Dr. Rehm said. VUS are often unavoidable because many variants are unique to individual patients, she noted, addressing the pros and cons of returning VUS results. While there are benefits, such as evidence-building, clinical follow-up, and informing decision-making, there can also be potential harms. VUS reporting can create patient anxiety, require additional health care resources, and even lead to mismanagement if a variant is misinterpreted.
“Clinicians make decisions every day in the face of uncertainty, but improved understanding of variants reduces the risk of harm and helps ensure the utility of genetic testing,” she said.
To improve understanding and resolution of VUS, improving standards for variant classification is a core focus. The draft Standards for Sequence Variant Classification v4.0 (SVCv4) represent a joint effort of the American College of Medical Genetics and Genomics (ACMG), Association for Molecular Pathology (AMP), College of American Pathologists (CAP), and Clinical Genome Resource (ClinGen). As an update to the 2015 ACMG-AMP standards, SVCv4 retains the major 5-tier scale from benign to pathogenic but adjusts the criteria for classification. “Among many adjustments to evidence scoring, it will become easier for variants to get to ‘likely benign,’ so the new standards will inherently reduce the VUS rate. This change is based on data on the direction of most VUS reclassification toward benign,” she explained.
The SVCv4 also subdivides VUS into 3 subclasses to help laboratories and clinicians interpret uncertainty more precisely. VUS-Low variants have minimal evidence of pathogenicity; VUS-Mid variants carry moderate uncertainty; and VUS-High variants show stronger evidence suggesting pathogenicity, warranting follow-up. According to Dr. Rehm, the subclasses “could be used to help labs decide which variants to report, guide clinicians on where to focus follow-up, and reduce noise from low-priority VUS while highlighting variants that could be clinically actionable.”
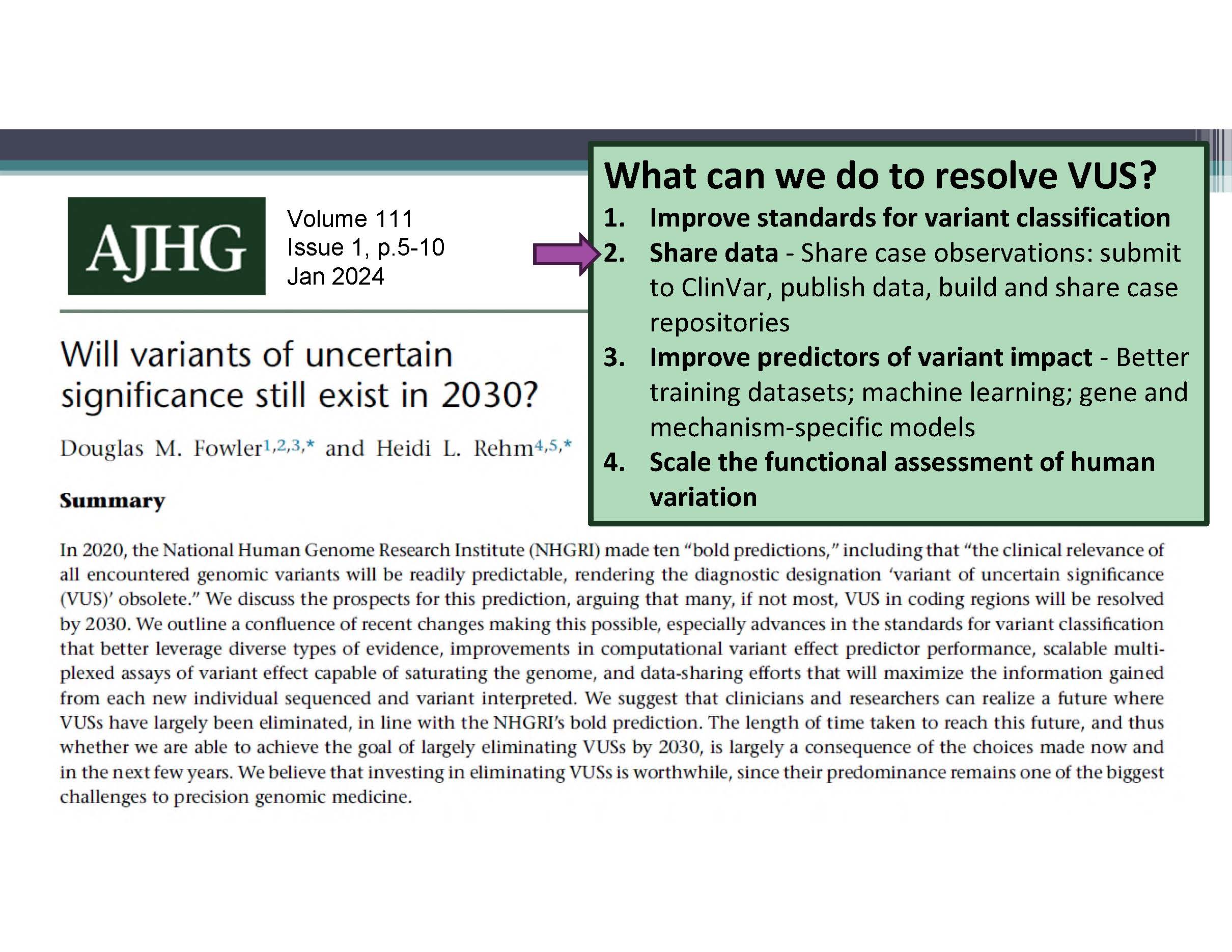
Dr. Rehm also discussed 3 other areas of focus to reduce the prevalence of VUS and improve the utility of genetic testing in clinical practice: robust data sharing, improved computational prediction, and scalable functional testing (Figure 1). Data sharing is essential to reclassifying VUS, she noted, as the failure to share information can cause “grave harms,” including misdiagnosis and unnecessary interventions. She highlighted initiatives like ClinVar submissions and public case repositories, and discussed future directions for gnomAD, including v5, which incorporates more than 415,000 genomes from the All of Us program, and v6, which will use federated aggregation to manage international data sharing requirements while improving allele frequency representation.
Improving predictors of variant impact is a growing area of computational genomics. Advances in machine learning and gene-specific or mechanism-specific models are enhancing interpretation of missense, indel, splice, and regulatory variants. Tools such as SpliceAI, Pangolin, PromoterAI, AlphaGenome and others are enabling labs to better estimate the functional effects of noncoding variants even in the absence of direct experimental evidence, she said.
Finally, scaling functional assessment of human variation is increasing the number of variants that can be directly tested in laboratory assays. Coupled with improved computational predictors, these scalable functional assays help move variants from uncertain to classified, enabling more actionable results for clinicians.